
Widely considered the “preeminent event for healthcare and wellness innovation,” HLTH was held in Las Vegas last month, and we couldn’t be more excited to share our experience. In summary, we believe we may be on the cusp of a transformative pivot – the dawn of a DIY healthcare revolution.
For the first time, it seems as if individuals will have the opportunity to truly “own” their healthcare experiences, thanks to emerging technologies that empower the diagnosis and self-monitoring of conditions from the comfort of home. I’m excited to share some technological marvels I witnessed at HLTH and how I believe they have the potential to reshape our healthcare ecosystem, making it more equitable, efficient, and patient-centric than ever before. As healthcare increasingly focuses on prevention rather than treatment, the patient journey is evolving into the integration of technology, data analytics, and value-based care. Here’s what the future may hold.
For patients with chronic conditions like Type II diabetes, conventional care involves daily glucose monitoring to regulate blood sugar levels. Additionally, bi-annual visits to a healthcare provider typically include lab visits, blood draws with results days later and medication adjustment guidelines from their doctor.
Imagine a different scenario: While shopping for dinner at your local grocery store, you use an automated blood-drawing kiosk by Truvian. In 30 minutes, your blood is drawn and processed, and results are sent directly to both you and your healthcare provider. A straightforward yet comprehensive report flags any alarming changes from your last test and suggests treatment adjustments if necessary. All of this is done asynchronously and independently by the patient, eliminating the need for a doctor’s direct involvement. The report and advice are generated by a medical board-certified AI bot.
I should note that I was able to test this technology myself – undergoing a blood draw and receiving my results while attending HLTH. I was shocked by the experience! The blood panel closely mirrored one I had recently completed at a doctor’s appointment, and the results were nearly identical. A significant difference between the two experiences: Truvian delivered results in 40 minutes, whereas it took days to get the same from my physician.
Arguably the most compelling aspect of this evolution is the democratization of healthcare. Cutting-edge innovations that make life convenient, such as Truvian’s mobile blood lab technology make crucial care accessible when and where people need it. In my opinion, of all the advancements showcased at the HLTH conference in Las Vegas, this is, hands down, the most thrilling.
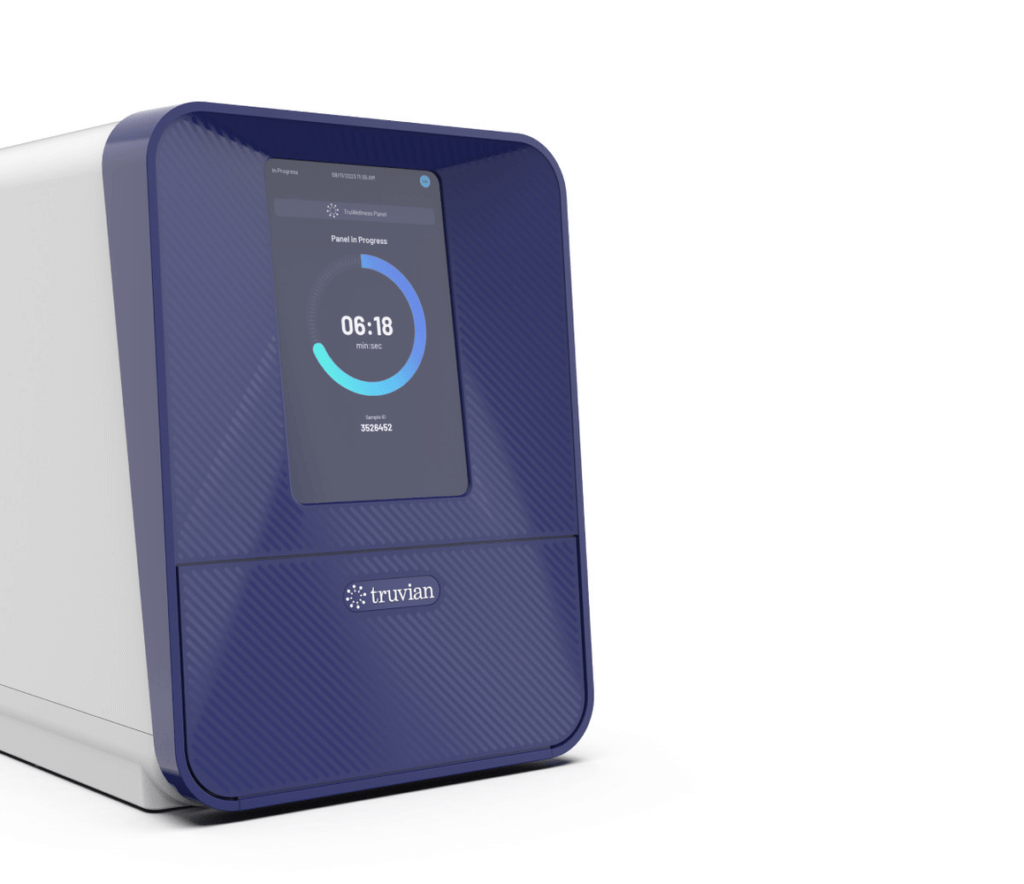
Truvian’s automated benchtop blood testing analyzer.
Another groundbreaking advancement: the “hospital at home” model. In the not-so-distant future, patients requiring more in-depth heart scans can manage the diagnostic process from home. QT Medical is developing a portable, disposable, and user-friendly test. Picture a band-aid-like application mailed to your home: You apply the device to your body which uploads your results to a cloud where it’s analyzed by AI. Patient and physician receive immediate results, charting out the next steps in a treatment plan, all without requiring a hospital visit. I believe this is more than mere convenience; it’s about extending the reach of healthcare, breaking down the barriers of geographic isolation and limited access to care.
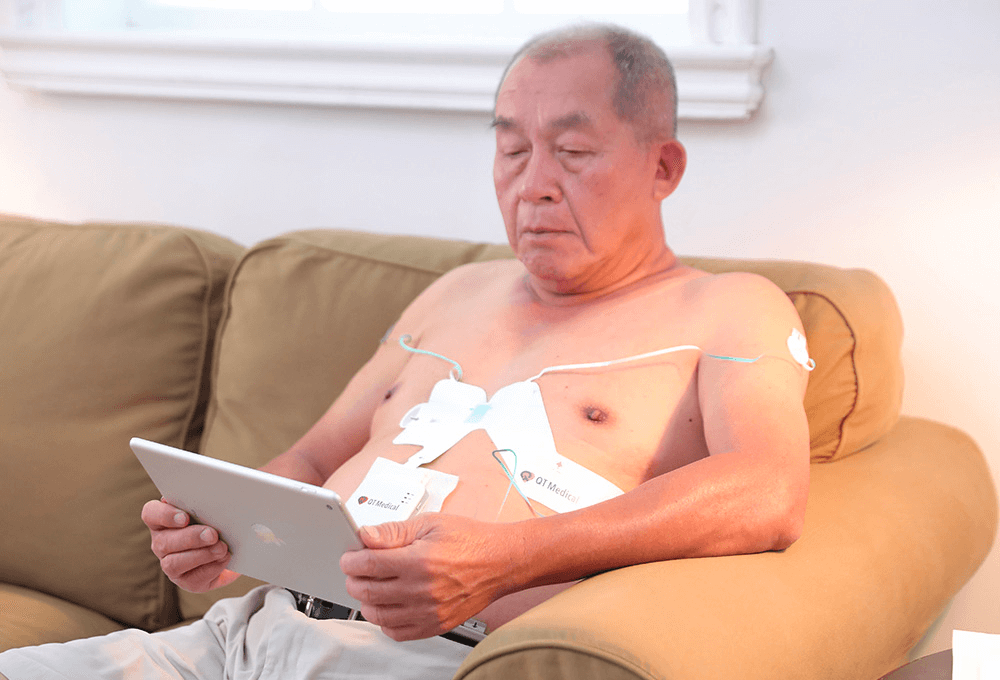
QT Medical’s PCA 500 12-lead resting ECG.
So many of our healthcare struggles stem from limited access to care. But what if all these data points could be logged into an integrated smart app, one that also tracks other health metrics? This would make remote patient monitoring not just possible, but effortless. Vital, a new API infrastructure company, promises to make this data interoperability possible.
The use cases mentioned above are just the tip of the iceberg. Here are just some possibilities on how remote monitoring and diagnostic technologies could redefine our healthcare journey:
Annual Physicals: An AI system could analyze previously documented patient notes, diagnoses, tests, lab results, etc., surfacing summarized information for clinicians to review prior to appointments.
Medication Refills: AI can review a patient’s medication history and vital signs, determining if a refill is warranted. Then, a second AI agent initiates an automated workflow to send the Rx request information to a digital pharmacy, which subsequently mails the prescription to the patient’s home.
Vaccine Visits: AI algorithms can identify the vaccines a patient requires, factoring in age, health conditions, and occupation. It can then coordinate with the patient to locate the closest vaccine administration site.
Chronic Condition Follow-Ups: For conditions like diabetes or hypertension, home-based A1C and ECG tests can be conducted. Data collected are reviewed by AI that flags any issues or discrepancies requiring medical intervention.
Minor Illnesses: For straightforward conditions like UTIs, imagine an at-home test kit that provides immediate results—akin to what Vivoo offers.
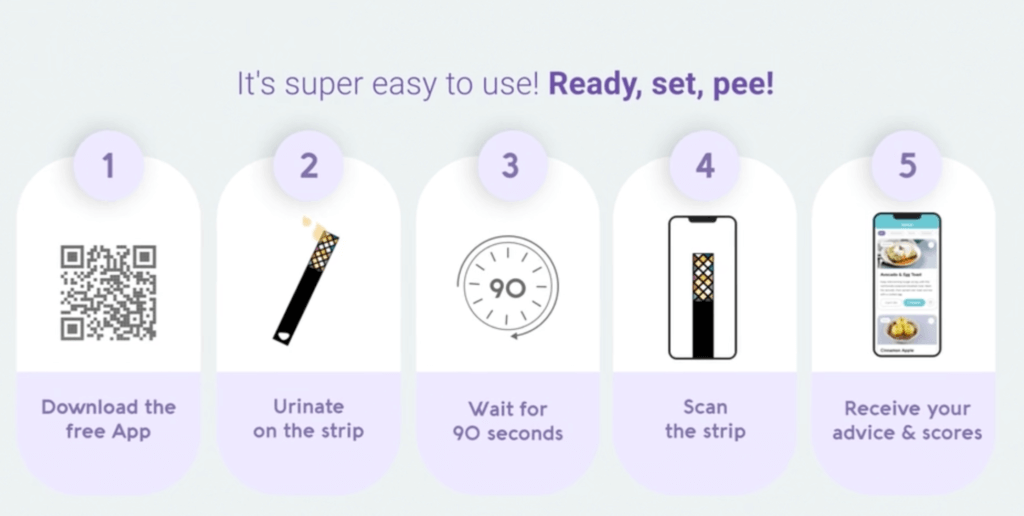
Vivoo provides immediate testing and results through a smartphone.
Other Health Screenings: For screenings related to cholesterol, cancer, and cognitive decline, new sensor technologies and medical devices are being developed to enable asynchronous diagnosis and monitoring at home. Currently in beta, Amissa collects biometric and behavior data from patient-worn Apple Watches and Fitbits to discover ways to prevent and delay the onset of Alzheimer’s disease and related dementias.
The patient journey of the future is a compelling vision of how technology, personalized care, and data analytics converge to create a healthcare system focused on prevention and value. It paves the way for increased efficiency, reduced healthcare costs, and—most importantly—one could say, a healthier, happier population. But as we prepare for this transition, the central tenet remains the same: a healthcare model where the patient is not just a recipient of care but an active participant in their own well-being.
